How long does it take to get pregnant after a vasectomy reversal? In this blog, we will explore the factors that influence the timeline for conception after a vasectomy reversal and provide a realistic outlook on what to expect. Deciding to undergo a vasectomy reversal is a significant step towards restoring fertility. However, one of the most common questions couples have is how long it will take to get pregnant after the procedure.

The Initial Healing and Recovery Period
Immediate Post-Surgery Recovery
After a vasectomy reversal, the body needs time to heal. The initial recovery period typically lasts a few weeks, during which patients are advised to avoid strenuous activities and sexual intercourse. This rest period is crucial to ensure proper healing and to reduce the risk of complications.
Resumption of Sexual Activity
Most doctors recommend abstaining from sexual activity for about two to three weeks after the surgery. This allows sufficient time for the surgical site to heal and for any swelling or discomfort to subside. Resuming sexual activity too soon can negatively impact the success of the reversal.
Factors Influencing the Time to Pregnancy
Sperm Return to Ejaculate
One of the primary factors influencing the time to pregnancy is the return of sperm to the ejaculate. This can vary widely among individuals. Some men may have sperm present in their ejaculate within a few months, while for others, it may take up to a year.
Age and Health of Both Partners
The age and overall health of both partners play a significant role in the time it takes to achieve pregnancy. Younger couples with good overall health typically have higher fertility rates and may conceive more quickly than older couples or those with underlying health issues.
Quality of the Sperm
The quality of the sperm, including factors such as sperm count, motility, and morphology, can impact the time to conception. It may take some time for the sperm quality to improve after the vasectomy reversal. Regular semen analyses can help monitor sperm quality and guide further treatment if necessary.
Frequency of Intercourse
The frequency of intercourse can also affect the time to pregnancy. Engaging in regular, well-timed intercourse around the woman’s ovulation period can increase the chances of conception.
Typical Timeline for Conception
While individual experiences can vary, here is a general timeline for what couples can expect after a vasectomy reversal:
- First 3 Months: Some men may have sperm return to their ejaculate within the first three months post-surgery. However, it is common for sperm count and quality to be low during this period.
- 3 to 6 Months: Sperm count and quality may start to improve. Couples may begin to achieve pregnancy during this timeframe, especially if the vasectomy reversal was performed within a few years of the original vasectomy.
- 6 to 12 Months: For many couples, this period is when the chances of achieving pregnancy are highest. Regular monitoring of sperm quality and maintaining a healthy lifestyle can support fertility.
- Beyond 12 Months: If pregnancy has not been achieved within a year, couples should consult their doctor to discuss further evaluation and potential treatments, such as assisted reproductive technologies (ART).
Monitoring Progress and Seeking Support
Regular Semen Analysis
Regular semen analysis is essential to monitor the progress of sperm return and quality after vasectomy reversal. This helps the doctor assess the success of the procedure and provide guidance on the next steps.
Emotional Support
The journey to conception after a vasectomy reversal can be emotionally challenging. It is essential for couples to support each other and maintain open communication. Seeking counseling or joining a support group can also provide valuable emotional support.
Pregnant After a Vasectomy Reversal: Conclusion
Achieving pregnancy after a vasectomy reversal requires patience and persistence. While the timeline can vary, understanding the factors that influence conception and maintaining a healthy lifestyle can improve the chances of success.
For expert guidance on vasectomy reversal and personalized care to support your fertility journey, contact:
Yaniv Larish, MD
4 East 76th Street
New York, NY 10021
Phone: (646) 862-5500
Dr. Yaniv Larish is dedicated to helping couples achieve their family planning goals through comprehensive care and support. Schedule a consultation today to learn more about the timeline for conception after vasectomy reversal and how to enhance your chances of success.


 Understanding whether health insurance covers vasectomy reversal in New York is a common concern for men considering this procedure, as costs can influence family‑planning decisions. While vasectomy reversal is a well‑established surgical option for restoring fertility, insurance coverage varies widely and depends on your plan, provider, and policy specifics.
Understanding whether health insurance covers vasectomy reversal in New York is a common concern for men considering this procedure, as costs can influence family‑planning decisions. While vasectomy reversal is a well‑established surgical option for restoring fertility, insurance coverage varies widely and depends on your plan, provider, and policy specifics.

 For couples hoping to conceive after a vasectomy reversal, a common question is: how long will it take to achieve pregnancy? While the answer varies depending on individual factors, understanding the typical timeline and influences on success can help set realistic expectations.
For couples hoping to conceive after a vasectomy reversal, a common question is: how long will it take to achieve pregnancy? While the answer varies depending on individual factors, understanding the typical timeline and influences on success can help set realistic expectations. For men considering a return to fatherhood after a vasectomy, vasectomy reversal can offer a hopeful path to natural conception. However, deciding whether it’s the right choice depends on several medical, emotional, and lifestyle factors. If you’re in the NYC or Tri-State area and weighing your options, this guide will help you ask the right questions before committing to surgery.
For men considering a return to fatherhood after a vasectomy, vasectomy reversal can offer a hopeful path to natural conception. However, deciding whether it’s the right choice depends on several medical, emotional, and lifestyle factors. If you’re in the NYC or Tri-State area and weighing your options, this guide will help you ask the right questions before committing to surgery.


 Vasectomy reversal is a highly effective and safe procedure, yet it remains surrounded by myths and misunderstandings. These misconceptions often deter men and couples from exploring the option of restoring fertility after a vasectomy. In this blog, we’ll debunk some of the most common misconceptions about vasectomy reversal to provide clarity for those considering the procedure.
Vasectomy reversal is a highly effective and safe procedure, yet it remains surrounded by myths and misunderstandings. These misconceptions often deter men and couples from exploring the option of restoring fertility after a vasectomy. In this blog, we’ll debunk some of the most common misconceptions about vasectomy reversal to provide clarity for those considering the procedure.
 Recovery after a vasectomy reversal is a crucial phase in the journey to restoring fertility, and understanding what to expect can significantly improve healing and long-term outcomes. While the surgical procedure itself is highly specialized, the post-operative period plays an equally important role in determining success. In this blog, we’ll cover recovery timelines, self-care tips, and what to expect during each stage of healing.
Recovery after a vasectomy reversal is a crucial phase in the journey to restoring fertility, and understanding what to expect can significantly improve healing and long-term outcomes. While the surgical procedure itself is highly specialized, the post-operative period plays an equally important role in determining success. In this blog, we’ll cover recovery timelines, self-care tips, and what to expect during each stage of healing.
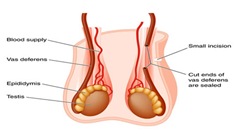
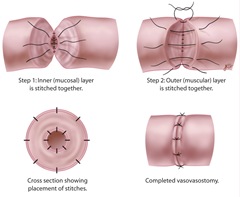
 In this article we’ll explore the importance of the surgical microscope in vasectomy reversal and how it contributes to optimal patient outcomes. Vasectomy reversal is a delicate procedure that requires extreme precision to reconnect the vas deferens and restore the flow of sperm. One of the most critical tools in ensuring a successful outcome is the surgical microscope. This advanced piece of technology allows urologic
In this article we’ll explore the importance of the surgical microscope in vasectomy reversal and how it contributes to optimal patient outcomes. Vasectomy reversal is a delicate procedure that requires extreme precision to reconnect the vas deferens and restore the flow of sperm. One of the most critical tools in ensuring a successful outcome is the surgical microscope. This advanced piece of technology allows urologic 
 Let’s explore the advantages and considerations of vasectomy reversal vs. IVF, helping you make an informed decision about the best route for your family planning goals. For men who have previously undergone a vasectomy but now wish to father children, two primary options exist: vasectomy reversal and in vitro fertilization (IVF). Both methods offer a pathway to conception, but they differ significantly in approach, cost, success rates, and long-term impact.
Let’s explore the advantages and considerations of vasectomy reversal vs. IVF, helping you make an informed decision about the best route for your family planning goals. For men who have previously undergone a vasectomy but now wish to father children, two primary options exist: vasectomy reversal and in vitro fertilization (IVF). Both methods offer a pathway to conception, but they differ significantly in approach, cost, success rates, and long-term impact. In in vitro fertilization (IVF), sperm is retrieved directly from the testicles through procedures like testicular sperm extraction (TESE) or percutaneous epididymal sperm aspiration (PESA). The retrieved sperm is then used to fertilize an egg in a laboratory setting, and the resulting embryo is transferred into the uterus.
In in vitro fertilization (IVF), sperm is retrieved directly from the testicles through procedures like testicular sperm extraction (TESE) or percutaneous epididymal sperm aspiration (PESA). The retrieved sperm is then used to fertilize an egg in a laboratory setting, and the resulting embryo is transferred into the uterus.

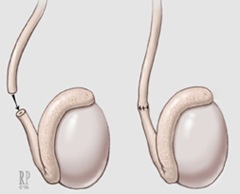
 What should you expect during a vasectomy reversal procedure? Vasectomy reversal is a highly specialized microsurgical procedure designed to restore fertility in men who have previously undergone a vasectomy. Whether due to changing life circumstances, a new relationship, or a desire to expand one’s family, vasectomy reversal offers hope to men seeking to father children again. Understanding the details of the procedure can help patients feel more confident about the process and what to expect.
What should you expect during a vasectomy reversal procedure? Vasectomy reversal is a highly specialized microsurgical procedure designed to restore fertility in men who have previously undergone a vasectomy. Whether due to changing life circumstances, a new relationship, or a desire to expand one’s family, vasectomy reversal offers hope to men seeking to father children again. Understanding the details of the procedure can help patients feel more confident about the process and what to expect.
 In this blog, we will explore various non-surgical alternatives to
In this blog, we will explore various non-surgical alternatives to