Vasectomy reversal is a highly effective and safe procedure, yet it remains surrounded by myths and misunderstandings. These misconceptions often deter men and couples from exploring the option of restoring fertility after a vasectomy. In this blog, we’ll debunk some of the most common misconceptions about vasectomy reversal to provide clarity for those considering the procedure.
Vasectomy reversal is a highly effective and safe procedure, yet it remains surrounded by myths and misunderstandings. These misconceptions often deter men and couples from exploring the option of restoring fertility after a vasectomy. In this blog, we’ll debunk some of the most common misconceptions about vasectomy reversal to provide clarity for those considering the procedure.
Myth 1: Vasectomy Reversal Is Never Successful
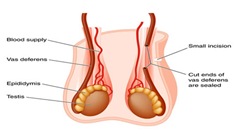
One of the most persistent myths is that vasectomy reversal doesn’t work. In reality, the success rate of vasectomy reversal is quite high—especially when performed by a skilled microsurgeon.
- Patency Rate: The return of sperm to the ejaculate occurs in approximately 70–90% of cases, depending on the time since the vasectomy.
- Pregnancy Rate: Successful pregnancies occur in 30–75% of couples after reversal, with higher chances when the female partner is younger and fertility is optimal.
Myth 2: It’s Only Effective If Done Within a Few Years
While it’s true that the best outcomes are often achieved when the vasectomy is reversed within 10 years, men have successfully undergone reversal even 15–20 years later.
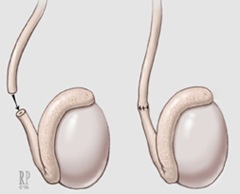
- Microsurgical Skill Matters: An experienced surgeon can address scar tissue and even perform a more complex procedure like a vasoepididymostomy when needed.
- Individual Factors: Success also depends on sperm quality, vasal fluid analysis, and the health of both partners—not just time.
Myth 3: Vasectomy Reversal Is Painful and Requires Long Recovery
Another misconception is that the procedure is extremely painful or involves a lengthy recovery. Most patients describe the discomfort as mild to moderate and manageable with over-the-counter pain medication.
- Outpatient Procedure: Vasectomy reversal is usually performed on an outpatient basis under general anesthesia.
- Recovery Timeline: Most men return to normal activities within 1–2 weeks, though strenuous activity and sexual activity are restricted for several weeks.
Myth 4: Reversal Always Requires IVF or Other Fertility Treatments
Some people mistakenly believe that vasectomy reversal needs to be combined with assisted reproductive technologies like IVF. In reality, the procedure is designed to restore natural fertility.
- Natural Conception: Once sperm is present in the ejaculate, couples can often conceive naturally without needing ART.
- Backup Options: If reversal is unsuccessful or if there are female fertility factors, sperm retrieval for IVF may still be possible.
Myth 5: Insurance Never Covers Vasectomy Reversal
While many insurance plans do not cover vasectomy reversal, some may provide partial or full reimbursement. It’s worth checking with your provider before ruling it out.
- Flexible Spending: HSAs and FSAs may be used to cover the cost.
- Consult Billing Specialists: Clinics can often provide documentation to help with insurance claims.
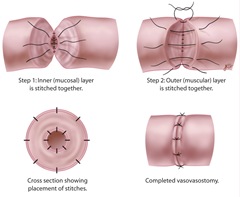
Myth 6: All Surgeons Offer the Same Level of Care
Not all urologists perform vasectomy reversals regularly, and not all are trained in microsurgery. Choosing a specialist with extensive experience in microsurgical vasectomy reversal can significantly improve your chances of success.
- Microsurgical Training: Look for a surgeon trained in using high-powered microscopes and fine suturing techniques.
- Case Volume: A surgeon who performs many vasectomy reversals per year is more likely to have refined skill and consistent outcomes.
Common Misconceptions About Vasectomy Reversal Conclusion: Separate Fact From Fiction
There are many misconceptions about vasectomy reversal that can discourage patients from considering the procedure. By separating fact from fiction and consulting with an experienced specialist, couples can make confident, informed decisions about their fertility future.
Schedule a Consultation
For personalized answers to your questions about vasectomy reversal and to explore whether it’s right for you, contact:
Yaniv Larish, MD
4 East 76th Street
New York, NY 10021
Phone: 646-862-5500
Dr. Larish offers expert microsurgical vasectomy reversal care with a focus on patient education and successful outcomes.